UCLA bioengineers and their colleagues have developed a smart insulin-delivery patch that could one day monitor and manage glucose levels in people with diabetes and deliver necessary insulin dosage. The adhesive patch, about the size of a quarter, is simple to manufacture and intended to work for 24 hours before needing to be replaced.
A study describing the research in which the patch was tested on mice and pigs was published in Nature Biomedical Engineering.
“Our main goal is to enhance health and improve the quality of life for people who have diabetes,” said study leader Zhen Gu, a professor of bioengineering at the UCLA Samueli School of Engineering. “This smart patch takes away the need to constantly check one’s blood sugar and then inject insulin if and when it’s needed. It’s mimicking the regulatory function of the pancreas, but in a way that’s easy to use.”
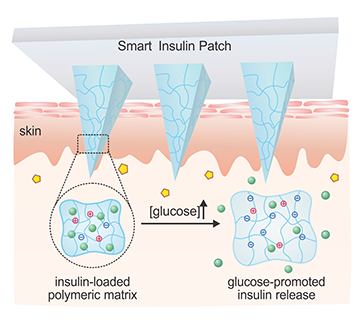
The smart patch monitors blood sugar (or glucose). It has doses of insulin preloaded in very tiny microneedles, less than 1 millimeter in length, that deliver the medicine quickly when the blood sugar levels reach a certain threshold. When blood sugar returns to normal, its insulin delivery also slows down. The researchers said the advantage is that it can help prevent insulin overdoses, which can lead to hypoglycemia, seizures, coma or even death.
“It has always been a dream to achieve insulin-delivery in a smart and convenient manner,” said study co-author Dr. John Buse, director of the Diabetes Center and the Translational and Clinical Sciences Institute at the University of North Carolina at Chapel Hill School of Medicine. “This smart insulin patch, if proven safe and effective in human trials, would revolutionize the patient experience of diabetes-care.”
Insulin is a hormone naturally produced in the pancreas. It helps the body regulate glucose, which comes from food-consumption and provides the body with energy. Insulin is the molecular key that helps move glucose from the bloodstream to the cells for energy and storage. Diabetes occurs when a person’s body does not naturally produce insulin (Type 1 diabetes), or does not efficiently use the insulin that is produced (Type 2). In either case, a regular dosage of insulin is prescribed to manage the disease, which affects more than 400 million people worldwide.
The treatment for the disease hasn’t changed much in decades in most of the world. Patients with diabetes will draw their blood using a device that measures glucose levels. They will then self-administer a necessary dose of insulin. The insulin can be injected with a needle and syringe, a pen-like device, or delivered by an insulin pump, which is a portable cellphone-sized instrument attached to the body through a tube with a needle on the end.
The microneedles used in the patch are made with a glucose-sensing polymer that’s encapsulated with insulin. Once applied on the skin, the microneedles penetrate under the skin and can sense blood sugar levels. If glucose levels go up, the polymer is triggered to release the insulin. The microneedle is smaller than a regular needle used to draw the blood, and it also does not reach as deeply so it is less painful than a pinprick. It penetrates about half a millimeter below the skin, which is sufficient to deliver insulin into the body.
In the experiments, one quarter-sized patch successfully controlled glucose levels in pigs with type I diabetes for about 20 hours. The pigs weighed about 55 pounds on average.
The technology has been accepted into the U.S. Food and Drug Administration’s Emerging Technology Program, which provides assistance to companies during the regulatory process. The researchers are applying for FDA approval for human clinical trials, which they anticipate could start within a few years. The team envisioned that the smart microneedle patch could be adapted with different drugs to manage other medical conditions as well.
At UCLA, Gu is also a member of the Jonsson Comprehensive Cancer Center, the California NanoSystems Institute and the Center for Minimally Invasive Therapeutics.
The study, supported by UCLA-based startup Zenomics, also included authors from North Carolina State University, the University of North Carolina at Chapel Hill, the Massachusetts Institute of Technology and Boston Children’s Hospital.
